What are the differences between magic mushrooms and ayahuasca? And what are the similarities between psilocybin mushrooms and ayhuasca? What is the difference in experience? And how do you know which one is better for somebody to choose?
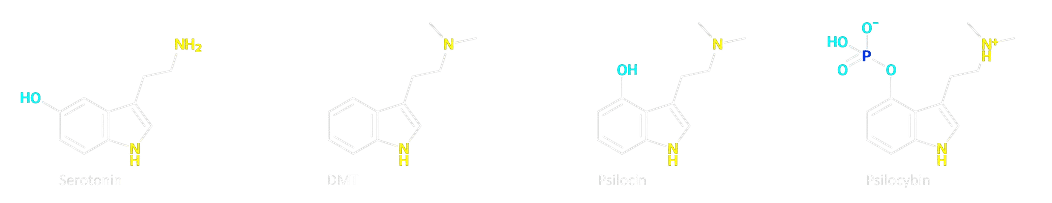
- Active Ingredients: Magic mushrooms contain psilocybin, which is converted into psilocine in the body, while ayahuasca contains DMT, which is often combined with a MAO inhibitor to prevent its breakdown in the digestive system.
- Preparation: Ayahuasca is a brewed drink made from various plants, while magic mushrooms are typically consumed whole or in tea form.
- Duration of Effects: The effects of ayahuasca can last 4 to 8 hours, while magic mushrooms typically last 3 to 7 hours.
- Psychedelic Effects: Both substances induce altered states of consciousness, visual and auditory hallucinations, and profound introspective experiences.
- Therapeutic Potential: Both have been studied for their potential in treating mental health issues such as depression, anxiety, and PTSD. Psilocybin seems to be a better choice in scientific literature.
- Serotonin Receptor Activity: Psilocybin and DMT both interact with serotonin receptors in the brain, leading to similar psychological effects.
- Intention: If seeking a deep spiritual journey or emotional healing, ayahuasca may be more suitable. For a lighter, more exploratory experience, magic mushrooms could be preferred.
- Setting: Ayahuasca ceremonies are often conducted in a group setting with a shaman, while magic mushroom experiences can be more flexible and done in various environments.
- Health Considerations: Consider any health issues, especially regarding MAO inhibitors, which are necessary for ayahuasca but not for magic mushrooms.
- Legality: In the Netherlands you can attend a psilocybin ceremony legally, but ayahuasca is illegal.
More information: Psilocybin (Mushrooms) | Ayahuasca
The choice between psilocybin mushrooms and ayahuasca represents not merely a selection between substances, but between distinct phenomenological landscapes, cultural paradigms, and therapeutic pathways. While both share the capacity to induce profound psychological transformation through serotonergic mechanisms, their differences in pharmacology, experiential trajectories, and cultural embeddedness create unique risk-benefit profiles.
Chemical Composition and Pharmacological Mechanisms
Psilocybin mushrooms primarily contain the prodrug psilocybin, which the body converts into its active metabolite, psilocin. Psilocin acts as a partial agonist at serotonin 2A (5-HT2A) receptors, modulating cortical activity and disrupting default mode network connectivity. This mechanism underlies the substance's ability to induce altered perception, ego dissolution, and mystical-type experiences.
Ayahuasca, by contrast, is a psychoactive brew traditionally prepared from the Banisteriopsis caapi vine and leaves of the Psychotria viridis shrubs. The brew contains N,N-Dimethyltryptamine (DMT), a potent psychedelic compound, and β-carboline alkaloids such as harmine and tetrahydroharmine. These β-carbolines function as monoamine oxidase inhibitors (MAOIs), preventing the enzymatic breakdown of DMT in the gastrointestinal tract and enabling oral bioavailability. The pharmacological synergy between DMT and MAOIs creates a unique pharmacokinetic profile distinct from psilocybin.
Receptor Affinity and Neurological Effects
Both substances primarily interact with serotonin receptors but exhibit different binding profiles. Psilocin shows high affinity for 5-HT2A, 5-HT2C, and 5-HT1A receptors, while DMT demonstrates broader activity at 5-HT1A, 5-HT2A/C, and sigma-1 receptors. The sigma-1 receptor modulation by DMT may contribute to ayahuasca's reported effects on cellular homeostasis and neuroplasticity.
The MAOIs in ayahuasca introduce additional neurochemical complexity. Harmine inhibits monoamine oxidase-A (MAO-A), increasing synaptic concentrations of serotonin, dopamine, and norepinephrine. This dual action—combining DMT's receptor effects with MAOI-mediated monoamine elevation—creates a neuropharmacological profile distinct from psilocybin's relatively selective serotonergic activity.
Temporal Dynamics and Phenomenology
Psilocybin experiences typically develop within 30–60 minutes of ingestion, peak at 2–3 hours, and resolve within 4–6 hours. Users frequently report vivid visual patterns, enhanced emotional sensitivity, and profound insights into personal or existential matters. The experience often progresses through distinct phases: initial somatic sensations, perceptual intensification, cognitive/emotional processing, and gradual return to baseline consciousness.
Ayahuasca ceremonies usually span 6–8 hours, with effects emerging within 30–45 minutes and peaking at 2–4 hours. The experience frequently includes intense visionary states, purgative effects (vomiting/diarrhea), and emotional catharsis. Unlike psilocybin's relatively smooth onset, ayahuasca often induces abrupt transitions between psychological states—a phenomenon colloquially termed "the launch".
Qualitative Differences in Consciousness Alteration
Comparative studies note distinctive experiential elements:
-
Visual Phenomena: Ayahuasca tends to produce more complex, narrative-driven visions compared to psilocybin's geometric patterns. DMT-induced visions often involve perceived interactions with autonomous entities or spiritual beings.
-
Emotional Processing: Psilocybin sessions frequently focus on autobiographical memory and emotional resolution, while ayahuasca experiences more commonly involve confronting existential or transpersonal themes.
-
Somatic Effects: Ayahuasca's physical effects are generally more pronounced, with 68% of participants reporting purging compared to 12% with psilocybin.
Mystical-Type Experiences
Both substances can induce mystical experiences characterized by unity, transcendence of time/space, and ineffability. However, ayahuasca users more frequently report encounters with perceived spiritual entities (87% vs. 49% for psilocybin), while psilocybin experiences more commonly emphasize interconnectedness with nature.
Therapeutic Applications and Clinical Research
Depression and Anxiety Disorders
Psilocybin-assisted therapy has demonstrated efficacy in treatment-resistant depression, with trials showing rapid antidepressant effects lasting up to 12 months. The COMPASS Pathways phase IIb trial found that a single 25mg dose reduced depression scores by -6.6 on the MADRS scale at week 3.
Ayahuasca shows promise for recurrent depression, particularly in treatment-refractory cases. A 2023 meta-analysis reported a large effect size (g = 1.25) for depression reduction post-ayahuasca session. The brew's MAOI components may enhance neurogenesis through increased brain-derived neurotrophic factor (BDNF).
Addiction and Substance Use Disorders
Ayahuasca has shown particular efficacy in addiction treatment. A Brazilian study of 194 participants with substance dependence found 69% remained abstinent 6 months after ayahuasca therapy. Proposed mechanisms include DMT-induced glutamate release in the prefrontal cortex and harmine's inhibition of dopamine reuptake.
Psilocybin research has focused on alcohol and tobacco addiction. A Johns Hopkins trial demonstrated that psilocybin-assisted therapy produced 83% smoking abstinence at 12 months—double the rate of standard treatments. The substance appears to facilitate behavior change by disrupting addictive neural circuits and enhancing cognitive flexibility.
PTSD and Trauma Processing
Ayahuasca's capacity to evoke intense emotional memories has led to its investigation for PTSD treatment. A 2024 trial with 65 PTSD patients found a 56% reduction in CAPS-5 scores after three ayahuasca sessions. Participants reported improved emotional regulation and reduced avoidance behaviors.
Psilocybin is being studied for end-of-life anxiety in terminal patients. A landmark 2024 study showed 78% of participants experienced clinically significant reductions in death anxiety persisting at 6-month follow-up. The substance's ability to facilitate acceptance of mortality appears linked to its induction of mystical experiences.
Cultural Contexts and Ceremonial Use
Traditional and Contemporary Practices
Ayahuasca use originates from Amazonian indigenous traditions, where it functions as a sacred medicine and diagnostic tool in elaborate ceremonies led by trained shamans. Modern ceremonies typically retain elements of this tradition—icaros (healing songs), dieta (dietary restrictions), and post-ceremony integration practices.
Psilocybin mushrooms have a more diverse ethnobotanical history, appearing in Mesoamerican rituals (e.g., Mazatec veladas) and contemporary Western therapeutic settings. Modern clinical protocols emphasize preparatory sessions, controlled dosing, and music-assisted psychotherapy.
Social Dynamics and Setting
The ceremonial context of ayahuasca creates distinct social-pharmacological interactions:
- Group Settings: 89% of ayahuasca ceremonies occur in groups, fostering collective energy and shared experience.
- Shamanic Guidance: Practitioners employ techniques like breathwork and energy cleansing to direct the experience.
- Post-Ceremony Diet: Traditional dieta restrictions (e.g., avoiding salt, sex, and stimulants) are believed to enhance spiritual receptivity.
Psilocybin therapy typically occurs in dyadic therapist-patient settings with eye shades and curated music playlists. This standardized approach facilitates reproducibility in clinical trials but lacks the cultural scaffolding of ayahuasca ceremonies.
Safety Profiles and Risk Considerations
Acute Adverse Effects
A comparative risk analysis reveals distinct safety profiles:
| Parameter | Psilocybin | Ayahuasca |
|---|---|---|
| Acute nausea | 44% | 92% |
| Vomiting | 12% | 68% |
| Transient hypertension | 18% | 51% |
| Anxiety/Paranoia | 31% | 29% |
| Prolonged psychosis* | 0.2% | 0.3% |
*In predisposed individuals
Ayahuasca's MAOI components introduce additional drug-drug interaction risks, particularly with SSRIs, stimulants, and tyramine-containing foods. Psilocybin has fewer pharmacological interactions but requires caution in patients with bipolar disorder or schizophrenia.
Long-Term Health Outcomes
Longitudinal studies of traditional ayahuasca users show improved cognitive flexibility and reduced psychopathology compared to controls. Chronic psilocybin use in non-clinical populations correlates with increased openness and nature relatedness. Both substances show low addiction potential, with dependence rates below 0.5%.
Guidance for Substance Selection
Decision-Making Framework
Choosing between psilocybin and ayahuasca requires evaluating multiple dimensions:
1. Therapeutic Goals
Psilocybin: Depression, end-of-life distress, smoking cessation
Ayahuasca: Addiction, PTSD, interpersonal trauma
2. Physiological Factors
Contraindications for ayahuasca: MAOI interactions, hypertension, cardiovascular conditions, psychosis
Psilocybin cautions: Bipolar disorder, acute psychosis, medication like Tramadol
3. Experiential Preferences
Ceremonial context vs. clinical setting
Tolerance for physical discomfort (purging)
Comfort with entity encounters vs. introspective journeys
4. Cultural Alignment
Resonance with Amazonian traditions or clinical psychotherapy
Importance of ritual elements vs. standardized protocols
5. Accessibility and Legality
Psilocybin decriminalization in select jurisdictions (legal in the Netherlands trough magi truffles)
Ayahuasca's limited legal protections under religious exemptions (illegal in the Netherlands)